NEMO Health and Availity integrate to deliver fully automated Clearinghouse Services with Revenue Cycle Management Workflow
A Combined Solution Simplifies Claim & Payment Processing
In a time of declining reimbursement and increased workload, finding ways to improve cash flow is more important than ever. NEMO Health and Availity Revenue Cycle Management (RCM) combine to deliver a solution that helps reduce denials and minimize days in accounts receivable. The result? Cleaner claims, fewer calls to the health plan, and faster payments.
NEMO Health and Availity RCM work seamlessly together to provide maximum convenience and flexibility by incorporating the following processes directly into your practice’s workflow:
TRANSITION FAQs
What is Availity?
Availity is NEMO Health’s new partnered clearinghouse.
What does Availity do that is different from Trizetto?
Availity has many features that we’re excited to use, here are a few:
- Much more robust reporting
- Corrections and Resubmissions through the web portal
- Pre-submission eligibility
- The ability to enable and disable front-end rejections at any time
- Secondary claim rules which will allow more efficient secondary claim turnaround
- Secondary claim submission directly through the web portal
Will this transition interrupt my cash flow?
No! Our developers have enabled us to submit claims to more than one clearinghouse during the transition. This means that even if enrollments are taking longer than anticipated, you will still be able to submit claims. EFT payments will not be interrupted.
How long will this take?
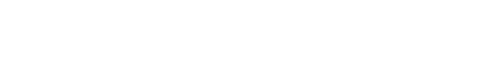
The major bulk of the transition will depend on payer approval of enrollments, which can range from 3 days to 8 weeks. The faster the enrollments are submitted, the faster the transition will go.
Can we begin submitting claims through Availity without all payers being approved?
Yes! Because our developers have created a way to submit to multiple clearinghouses, we can begin submitting claims to Availity at any time.
What if we need to add a payer after the transition is finished? Whom do we contact?
Availity can help provide you with the necessary instructions.
Why do I see the same ERAs available on both Availity and Trizetto?
During our beta testing, we found that in a handful of cases some payers were sending remits to both clearinghouses at once. The remits will eventually drop off of Trizetto so that they can be disregarded.
I submitted enrollment forms to Availity, and suddenly my claims for Medicare are being rejected in Trizetto, why is this happening? What should I do?
During our beta testing, we found that some users submitted their Medicare enrollment with “Single Submission” selected. This will limit you to submit claims through only one clearinghouse. We suggest selecting “Dual Submission” so you can submit through both clearinghouses. Contact Availity to see if you can begin submitting your claims through Availity instead. Alternatively, you can resubmit your enrollment paperwork with “Dual Submission” selected.
Can I submit claims to more than one clearinghouse (ie, Trizetto and Availity)?
TRAKnet has been programmed to allow for submission of claims and downloading of remits to both Availity and Trizetto clearinghouses at the same time. Here is a quick explanation on how it works:
- Inside of TRAKnet there is a toggle that will allow you to designate whether an insurance is enrolled through Availity or Trizetto. By default the insurances will be set to Trizetto. This can be changed in two ways:
- Individually: By going to Properties->Insurances->Search for an insurance and open it. At the bottom of the General tab there is a setting that can be switched between Availity and Trizetto.
- All at once: By going to Properties->Insurances->Clearinghouses. At the bottom of the tab you will see a button for changing all insurances to Availity or Trizetto, depending on which tab you have selected.
After making that change, and verifying you have the correct information listed in the FTP settings found in Properties->insurances->Clearinghouses, you will just submit claims normally. The process for submitting claims is exactly the same. When you send out a claim TRAKnet will review the insurance specific settings and send it to the correct clearinghouse.
Downloading remits is just as easy. The only setting you will want to verify is under Properties->Insurances->Clearinghouses->Availity-> change Use Test Environment = False. Be sure to verify that Availity has moved your office into production before continuing. After that is set up you will simply need to go to either Trizetto or Availity, select the remits you want to download, and then under Billing Dashboard->Claims select “Receive.” TRAKnet will check both Trizetto and Availity for any downloaded FTPs and then bring them into the system to post.
Does NEMO Health or Availity help with credentialing?
No, this is not a service that we currently offer.